Background
The fast development of computer and Internet technology has facilitated the revolution of medical education. Nowadays, more and more medical schools around the globe choose to use online teaching websites to set courses as complementary tools for helping students study. The Ministry of Education in China initiated the Education Informatization Plan 2.0 in 2018, which stepped up the transition of education. The covid-19 pandemic and the quarantine measures taken by the Chinese government in 2020, all of a sudden, accelerated the transformation of online education. All universities, including medical schools, were forced to use online teaching tools overnight. Though harrowing for some of the Chinese medical schools, the transition of teaching methods has succeeded and even popularized after the containment of the virus.
Faced with this dramatic shift to online medical education, researchers of different countries conducted surveys from various perspectives. New findings such as a significant difference between students’ and lecturers’ opinions on the optimal amount of online learning were helpful for the improvement of online education.1 Studies also found that online education could improve critical thinking ability and knowledge application beyond physical classroom boundaries.2 However, there are also many shortcomings in online medical education. Regarding asynchronous online education which is a mode widely adopted in China, teachers’ concern about students’ understanding of the concepts and whether the teachers checked students’ understanding were two common shortcomings.3 What is online medical education efficacy evaluation of the teachers and students? That might be a crucial question. It is widely acknowledged that one of the most significant disadvantages of online teaching is the explanation of practical concepts.4 Limited interactions and technical difficulties were concerned by many researchers.5 Lack of direct teacher-student contact and interactions among students themselves will affect the understanding of practical concepts and the perception of learning during the course negatively.6 The efficacy of practical online courses, therefore, might be an essential issue. When learning online at home, students are often unsupervised by teachers if the courses were not live-stream. Can parents take on the responsibility of the teachers? That is unknown to the researchers. To optimize medical education in the future, it is imperative for researchers to understand the status of online medical education in China and identify online teaching and learning challenges.
There was also a dearth of papers exploring the perception between teachers and students on online medical education. Although the pandemic boost the development of online medical education and numerous researchers studied the topic, studies focusing on online teaching still lack attention. Online medical education was a comparatively new concept, and it was implemented overnight due to the strict quarantine measures taken by the Chinese government. Challenges would pop up one by one as time went by due to the quick decision and unprepared schools. However, many surveys of this kind were distributed to students for one time without identifying the changes during the dramatic shift to online medical education. Therefore, the authors conducted three massive surveys in different phases to identify the challenges that would not be found out for just one survey to offer insight into the popularization of online medical education. The aim of the conducted four surveys was trying to find out problems that matter and possible solutions from the perspective of students and teachers on online medical education, which may enlighten future related studies in China or other developing countries.
Methods
Participants
All experimental protocols of the study were approved by the Board of Academic and Teaching Affairs of Nanjing Medical University and conducted by the Institute of Medical Education of NMU. All respondents were undergraduate students and teachers who were over 18 years old, and informed consent was obtained from all subjects. Demographic descriptions of respondents of four surveys are shown in Table 1. The informed consent was shown before the survey, and respondents filled out the surveys if they wanted to. If respondents were unwilling to join the research or wanted to stop during the survey, they could choose to close the app to quit the survey. Surveys were distributed and collected on the survey system of NMU on the cellphone app named WeChat and the questionnaire website named Wenjuanxing (www.wjx.cn). At that time, face-to-face classes were entirely replaced by online education in China. Institute of Medical Education contacted its counterparts from other schools in China and distributed the surveys for students on February 17 (the first day), February 25 (the first week), and March 20 (the first month). And then, the undergraduates in these schools participating in online education were recruited in this survey. The survey for teachers was also conducted on March 20 in the same way, which was distributed by our counterparts to the teachers teaching undergraduate online medical courses. Teachers who received invitations would choose to answer the survey of their will. Students and teachers could participate in the survey anonymously to ensure that they could express true thoughts. The questionnaires were conducted online by the researchers.
|
Table 1 Demographic Description of the Respondents |
Questionnaire
Four structured and self-administered questionnaires were developed consisting of questions that mainly covered: (1) rate of satisfaction for online education; (2) significant problems and obstacles of online teaching and learning; (3) assessment of online teaching and learning and comparison to face-to-face classes; (4) follow-up measures that need to be taken. (5) other critical issues related to online medical education. The questionnaires were all in Chinese, and no time limit was required. At first, the author studied and designed the original Questionnaires. Then, the questionnaires would be piloted among 20 volunteers recruited randomly and modified according to the pilot results to avoid ambiguous content and other problems. At last, questionnaires would be validated and scrutinized by the Board of Academic and Teaching Affairs of Nanjing Medical University before massive distribution.
Data Analysis
Percentage was calculated according to the number of respondents per response in relation to the number of total responses of a question. Reliability and validity tests were run before analyzing. The collected data were analyzed on the software named SPSS.
Results
Survey for the Students in Phase One
After the swift decision of shifting to online medical education overnight, we wanted to have the first understanding of the implementation of online theoretical medical education. Researchers collected 2378 undergraduate medical students’ results except for clinical students who were due to accepting practical training in the fifth year. The reason for not collecting students in the clinical phase was that the large-scale practical courses were not initiated. Demographic descriptions of the respondents in the first survey can be seen in Table 1. At that time, 99.75% of the surveyed students participated in online learning. Most students were satisfied with teaching management, pedagogy, resource, and online interaction. However, when it came to the learning efficacy of online theoretical education, the satisfaction rate dropped sharply (Table 2). As for the most used online learning platform, Chaoxing learning platform (www.chaoxing.com) was used by 30.68% of the students, making it the most welcoming platform.
|
Table 2 Percentage of Satisfaction of Online Medical Education |
Survey for the Students of Clinical Medicine in Phase Two
After mastering the basic situation of online theoretical learning, researchers of IME surveyed undergraduate students studying clinical medicine. Authors collected 995 responses. The demographic description can be seen in Table 1. Most surveyed students had good Internet connections to learn online. Only 1.91% of students neither had good WIFI connections nor cellphone connections, making it hard for them to study online.
First, as for the equipment, 52% of the students chose to use computers, and one-third of the students would use the pad to learn online. Only about one-fifth of the students would use cellphones to learn online. Second, as for the learning experience before the massive shift to online learning, 32% of students never used online learning sources before. That meant they were unfamiliar with online teaching resources such as MOOC. Third, when speaking of the most popular learning resource website, 40% of the Chinese students watched learning videos on the video website called Bilibili (www.bilibili.com) to assist them in learning online. Fourth, most students worried that the content was hard learn online when it came to the most worrisome aspect. Concerning the real problems that happened during online learning, most students encountered network connection pressure (Table 3). Fifth, in terms of online satisfaction rate, the least satisfying aspect of learning online was the interaction with the teacher.
 |
Table 3 Worrisome Aspect and Challenges for Students of Clinical Medicine Studying Online |
Students who were scheduled to be trained in the hospitals have to watch videos and read case reports online due to the quarantine measures. They thought that online learning was necessary, but it was not suitable for every type of learning. For the students, online learning seemed more suitable for preclinical students who were taught theoretical courses. Most students thought that practical courses online could not meet their learning needs. Opinions on the efficacy of online Problem-Based Learning, Case-Based Learning, and Team-Based Learning were divided (Table 4). For the clinical students surveyed, the least satisfying aspect was also the interaction and answering questions online.
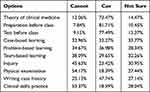 |
Table 4 Whether Online Clinical Teaching Could Meet Different Learning Needs |
Survey for the Students in Phase Three
After roughly a month of online learning, researchers intended to survey the implementation status again and collected 8058 responses for the third survey. Demographic descriptions can be seen in Table 1. As for the learning conditions, the results showed that 98.85% of students had Internet connections which was a rise compared with the survey in phase two. 98.46% of students had online learning equipment. 62.42% of students like to learn on the laptop, which was a rise compared with the survey in phase two. Most parents (40.74%) would supervise their children’s online learning from time to time, while 39.87% of parents often did that. Only 19.39% of parents would not check it at all.
First, when it comes to the curriculum, the results showed that students learned 8.63 courses online on average, including 7.31 compulsory courses and 1.32 elective courses. The best-done aspect was that four-fifths of the courses had homework. As for the shortcomings, different from what was implemented in many developed countries, most surveyed students did not have live-stream classes online. This kind of class only accounted for 12.4% of the classes, and this situation was even worse for the elective courses. Another particular problem was that only 36.27% of the courses had a quiz (Table 5).
 |
Table 5 Perceptions on Online Learning |
Second, 61.51% of the students thought that online medical education could not meet their needs to master compulsory courses. Face-to-face classes explaining complex parts of compulsory courses may be necessary, while in-person classes of elective courses were the other way around.
Third, as for the most significant challenge after learning online for a month, the biggest problem was learning motivation (Table 6). Percent of the lagging platform and poor interaction surveyed in phase two, which was deemed the main challenge seemed to drop a lot in phase three.
 |
Table 6 The Biggest Challenge of Learning Online After a Month |
Survey for the Teachers
After the first month of online teaching, researchers also distributed surveys to teachers and collected 575 responses. The disciplinary background of the teachers is shown in Table 1. Generally speaking, 66.73% of teachers taught one course online, and only 2.93% of teachers taught more than three courses. As for the teaching equipment, the investigation showed that 96.52% of teachers would use the computer to teach, and 42.26% of teachers would use the cellphone to teach. Computer and cellphone was the leading teaching equipment instead of the pad and other gadgets. 62.96% of teachers chose the teaching platform as the primary communication software.
In terms of online teaching implementation, more than 90% of teachers responded that they had told students the teaching objective, offered learning resources, given assignments, and interacted with them. During online medical education, 69.27% of the surveyed teachers chose to change or use more learning platforms online. Speaking of the reason for switching platforms, teachers tended to use platforms with more available functions (Table 7).
 |
Table 7 The Reason of Changing or Adding Teaching Platforms |
When asked whether it is necessary to re-teach the class face-to-face after the online education, the answer seemed to differ dramatically. Necessity to reteach in-person from top to bottom was recognized by only 2.39% of the teachers. 44.22% of teachers said they only need to focus on explaining part of the chapter content or arranging Q&A classes. 49.91% of teachers thought that there was no need to teach the lesson face-to-face again.
Discussion
Generally speaking, the surveys have shown that the online medical education implemented in China went smoothly and was satisfying, although shifting to online education was abruptly. The progression of online medical education revealed by the investigation seemed to be better than what the researchers imagined. In terms of learning conditions and environment, most students had Internet connections and equipment to study online. Regarding the home learning environment, most parents would remind their children to study at home – at least from time to time. Some researchers found that due to Chinese parents’ lack of time and professional knowledge, they were neither trained nor ready to embrace online learning.7 Reminding their children, as the author assumed according to that conclusion, might be one of the few things that Chinese parents would do. As for problems, the major challenge was hardware issues such as the lagging platform and problems arising from the unfamiliarity of teachers, such as the lack of interaction. However, as time went by, the biggest challenge seemed to be the learning motivation because they are learning at home – a place with less supervision than schools. Another significant finding was the sharp difference between teachers and students over the online education efficacy evaluation. When asked if the respondents need in-person classes as a supplement after the quarantine ended, most students responded that they need face-to-face classes because online learning did not meet their needs. Oppositely, most teachers responded that in-person classes after the quarantine to explain the online courses’ knowledge were unnecessary because they thought online education had reached teaching objective.
When it comes to implementing online medical education, infrastructure, including learning equipment and Internet connection, was one of the major challenges in developing countries.8 However, that challenge was the original one for medical students learning online in China and was soon replaced as the issue was fixed in a short time. The operation of online learning websites and apps took tremendous pressure because the whole country started online education overnight, which generated numerous pressure on servers. Thanks to the high work efficiency of the platform companies, students’ learning motivation, however, replaced the problem of platforms’ operation, becoming the biggest challenge for students learning online. The result was similar compared with other massive surveys in China.9 Therefore, for other developing countries, the construction of infrastructure is vital for promoting online medical education, especially the Internet server construction of the teaching platforms. Medical education on the Internet may not be popularized in most developing countries, but infrastructure construction could be done ahead of the transition. For the developed countries in which online medical education has already become mainstream, students’ learning motivation should be taken seriously. Students’ motivation was all likely to be affected by their environment.10 As is shown in the results, not all the parents would remind their children to study all the time. An effective supervision system on the Internet or the help from parents at home is worth exploring to enhance online learning efficacy better.
Researchers found interesting results after comparing the results of students’ surveys with teachers’ surveys. The first one is the need for in-person classes to re-teach. Most students thought it necessary to have the in-person classes again, especially for the compulsory courses, while nearly half of the teachers thought there was no need to explain the knowledge to the students again face-to-face after quarantine ended. The reason that caused this sharp difference might derive from flawed online education assessment system and lack of the concept of formative evaluation. According to the research, only one-third of the online classes had quizzes. Most Chinese college teachers still implement the strategy of conclusive evaluation, which means that the final is the only test deciding a student’s performance in the whole semester. This teaching strategy brought online may lead to a wrong evaluation result from the teacher. Some researchers in developing countries thought that assessment via relatively unfamiliar methods and environments is challenging to both the students and examiners.11 However, studies have shown that medical students find online formative assessments helpful for their learning.12 Therefore, some researchers suggested that it is vital to construct an online education assessment system.13 A scientific mechanism monitoring online students can boost students’ learning motivation when studying alone and give teachers feedback so that they can understand the efficacy of the class. Besides this, we should note that a formal evaluation process might discourage active student participation.13 No studies focusing on online education efficacy evaluation tools have been found. However, we should be aware that the evaluation tools need to adequately address learning outcome which is closely related with teaching quality.14 The real reason leading to the different perceptions of online education effect is complex for sure. More related research should be done to find out more.
The second one is the satisfaction of online interaction. Online learning might not compete with offline learning in terms of interactive knowledge building between teachers and students.15 According to the survey, 94.26% of teachers said they interacted with the students online, while 57.94% of the students thought online interaction was not enough in phase three. Students in one-to-one online meetings often seem relaxed and open.16 That might be the solution because relaxed and open students may tend to interact with the teachers.
The third one is the use of online education technology by teachers. With the development of 5G and other technologies, new forms of online teaching are springing out, but teachers in China did not get used to them. According to the research, only 12% of the courses were taken through live-stream. Most teachers chose to let the students watch videos instead of teaching them in person online. Teachers could not perceive whether the students got it by detecting expressions on the students’ faces on the Internet. Hence, faculty training for the implementation of new education technologies is of vital importance.17 In developed countries such as Italy, teachers’ limited skills to use technology were one of the major weaknesses of online medical education.18 China was no exception. Numerous teachers in China still could not utilize different kinds of online education tools proficiently. The majority’s concept of online education was limited to watching videos and assignments online. Educating teachers to transform the idea is essential for medical schools in China.
Not all the content was suitable to be taught online, according to the students. Online medical education was suitable for theoretical teaching, preparation for the class and test. Uploading learning materials online will assist most students to understand the content better. Although some researchers thought that a significant shortcoming of e-learning technologies had been poor support for group-oriented learning,19 the opinions of the surveyed students were divided. Communicating and collaborating were feasible on the Internet, but they were not sure whether they could achieve the goal of the class. When discussing applying current education forms to practical courses such as physical examination and clinical skills practice, most students were against the idea. Watching videos and reading requirements can not help the students in terms of practical skills. Medical simulation technologies such as VR and in-site training may be indispensable for clinical students. Emerging technology, though it may act as a servant of a disruptor sometimes,20 is a promising way of teaching practical courses online. A mixture of online and in-person teaching incorporated into these effective learning methods would be a direction in the future.21
Conclusion
Our findings demonstrated that online medical education in China was implemented smoothly yet with many issues left to be resolved. The changing challenge during the implementation of online medical education manifests that the infrastructure was the prerequisite for the implementation, and a scientific mechanism monitoring online students may be crucial for a better online medical education. Besides this, faculty training and emerging technologies are also promising ways of improving online medical education. Such measures will help narrow the difference between teachers and students in terms of online education evaluation and provide guidance for online medical education in the future.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Please contact the corresponding author or the first author and state the purpose if one need the original data and should be aware that the original data are written in Chinese.
Ethics Approval and Consent to Participate
Ethical approval for this study was obtained from the Board of Academic and Teaching Affairs of Nanjing Medical University. The work was carried out in accordance with the Declaration of Helsinki. Participants took the survey anonymously, so their personal information was protected. A consent declaration was presented before the survey, and informed consent was obtained from all subjects. Once starting the survey, participants can withdraw consent by closing the app or website, and no data will be collected. As no identifiable data is collected, participants will not be able to withdraw consent following completion of the survey unless they have chosen to contact distributors or Nanjing Medical University at the end of the survey.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Schlenz MA, Schmidt A, Wstmann B, Krmer N, Schulz-Weidner N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): a cross-sectional study. BMC Med Educ. 2020;20:354. doi:10.1186/s12909-020-02266-3
2. Lahti M, Kontio R, Pitkänen A, Välimäki M. Knowledge transfer from an e-learning course to clinical practice. Nurse Educ Today. 2014;34(5):842–847. doi:10.1016/j.nedt.2013.09.003
3. Jayathirtha G, Fields D, Kafai YB, Chipps J. Supporting making online: the role of artifact, teacher and peer interactions in crafting electronic textiles. Inf Learn Sci. 2020;121(5/6):371–380. doi:10.1108/ILS-04-2020-0111
4. Sankaranarayanan S, Kandimalla SR, Cao M, Maronna I, An H. Designing for learning during collaborative projects online: tools and takeaways. Inf Learn Sci. 2020;121(7/8):569–577. doi:10.1108/ILS-04-2020-0095
5. Knipfer C, Wagner F, Knipfer K, Millesi G, Nkenke E. Learners’ acceptance of a webinar for continuing medical education. Int J Oral Maxillofac Surg. 2019;48(6):841–846.
6. Fulton C. Collaborating in online teaching: inviting e-guests to facilitate learning in the digital environment. Inf Learn Sci. 2020;121(7/8):579–585. doi:10.1108/ILS-04-2020-0116
7. Dong C, Cao S, Li H. Young children’s online learning during COVID-19 pandemic: chinese parents’ beliefs and attitudes – ScienceDirect. Child Youth Serv Rev. 2020;118:105440.
8. Nimavat N, Singh S, Fichadiya N, Sharma P, Pandit N. Online Medical Education in India – different challenges and probable solutions in the age of COVID-19. Adv Med Educ Pract. 2021;12:237–243. doi:10.2147/AMEP.S295728
9. Wang K, Zhang L, Ye L. A nationwide survey of online teaching strategies in dental education in China. J Dent Educ. 2021;85(2):128–134.
10. Binks AP, Leclair RJ, Willey JM, Brenner JM, Schwartzstein RM. Changing medical education, overnight: the curricular response to COVID-19 of nine medical schools. Teach Learn Med. 2021;6:1–9.
11. Sigdel S, Ozaki A, Dhakal R, Pradhan B, Tanimoto T. Medical education in Nepal: impact and challenges of the COVID-19 pandemic. Acad Med. 2021;96(3):340–342.
12. Snekalatha S, Marzuk SM, Meshram SA, Maheswari KU, Sugapriya G, Sivasharan K. Medical students’ perception of the reliability, usefulness and feasibility of unproctored online formative assessment tests. AJP Adv Physiol Educ. 2021;45(1):84–88. doi:10.1152/advan.00178.2020
13. Jeong HC, So WY. Difficulties of online physical education classes in middle and high school and an efficient operation plan to address them. Int J Environ Res Public Health. 2020;17(19):7279. doi:10.3390/ijerph17197279
14. Schiekirka S, Reinhardt D, Heim S, et al. Student perceptions of evaluation in undergraduate medical education: a qualitative study from one medical school. BMC Med Educ. 2012;12(1):45. doi:10.1186/1472-6920-12-45
15. Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538. doi:10.1080/10872981.2019.1666538
16. Browne J. “Excuse the cat … ” Reflections on online mentoring during the COVID‐19 pandemic. Med Edu. 2021;55(6):673–675.
17. Farooq F, Rathore FA, Mansoor SN. Challenges of online medical education in Pakistan during COVID-19 pandemic. J Coll Physicians Surg Pak. 2020;30(6):67–69.
18. Consorti F, Kanter SL, Basili S, Ho MJ. A SWOT analysis of Italian medical curricular adaptations to the COVID-19 pandemic: a nationwide survey of medical school leaders. Med Teach. 2021;20:1–8. doi:10.1080/0142159X.2021.1959024
19. Franceschi KG, Lee RM, Hinds D. Engaging E-Learning in Virtual Worlds: Supporting Group Collaboration. Hawaii International Conference on System Sciences. IEEE. 2008(1):7.
20. Hays RB, Ramani S, Hassell A. Healthcare systems and the sciences of health professional education. Adv Health Sci Educ. 2020;25(5):1149–1162. doi:10.1007/s10459-020-10010-1
21. Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):42378. doi:10.1136/bmjopen-2020-042378
